You are probably wondering why you are in a plastic surgeon’s office when you have a diagnosis of breast cancer. Some plastic surgeons devote a substantial part of their practice to making the treatment of breast cancer easier by offering breast reconstruction surgery to women who require mastectomies. Reconstructive surgery in this setting is different than cosmetic surgery. It is about trying to make the patient feel whole again. It can enable her to regain control of her life. So much of breast cancer treatment is dictated to a patient by the stage of her disease. Breast reconstruction can give a woman a voice in her treatment: does she want reconstruction? If so, how and when? You had no choice in having breast cancer, but you do have some say in how you to choose to respond to it.
The Breast Cancer Treatment Process
Step One:
First, a biopsy is done to establish that you definitely have breast cancer. You most likely have already had a breast biopsy, which demonstrated that you have either non-invasive (in situ) breast cancer or invasive breast cancer. Non-invasive breast cancer means the tumor is still in your milk ducts, and cannot have already spread elsewhere. Invasive breast cancer has usually originated in the milk ducts and has penetrated the wall of the duct and moved into the surrounding breast tissue. These cancers can be treated with either a lumpectomy and radiation or with a mastectomy; your survival would be the same with either treatment. If you are being advised to have a mastectomy, it is generally because your tumor is too large, relative to the size of your breast, to be adequately removed and leave your breast with an acceptable cosmetic result. Some patients who would otherwise be poor candidates for lumpectomy can be converted into good candidates by having an Oncologic Breast Reconstrution (see below.) Alternatively, you may not wish to have a lumpectomy and radiation, and therefore you have chosen a mastectomy by default in that you do not wish to have lumpectomy followed by radiation.
Step Two:
Invasive cancer can spread, and if it was found in your initial biopsy, you may have a separate outpatient procedure known as a “sentinel node biopsy” to see if the cancer has spread to the lymph nodes in your axilla (armpit). If it has, additional lymph nodes may be removed during your mastectomy. This finding will also mean you will definitely need chemotherapy after your mastectomy.
Step Three:
This step begins with either a lumpectomy or a mastectomy. If it is a simple lumpectomy, it will be done solely by your breast surgeon. If it is a complicated lumpectomy, the plastic surgeon will perform an “Oncologic Breast Reconstruction” immediately following your lumpectomy (again, see below).
Alternatively, you will proceed with a mastectomy. In a “skin-sparing mastectomy” the entire breast is removed along with the nipple and areola, and no other skin is removed. If your tumor is a more favorable size and location, you may be eligible for a “nipple-sparing mastectomy,” which removes the entire breast but leaves the nipple and the areola. Learn more about “Nipple-Sparing Mastectomy“. Both of these procedures are called a “simple mastectomy” or a “total mastectomy”. If you had a positive sentinel node biopsy, you will have additional lymphatic tissue removed from your axilla, making this procedure a “modified radical mastectomy”. You may have heard the term “radical mastectomy”. This refers to a procedure where the breast, lymphatic tissue, and pectoralis major muscle are removed. This procedure was common at one time, but research has shown it offers no treatment advantage and is therefore seldom performed.
If you choose to have breast reconstruction, the first phase is frequently begun right after the mastectomy and is therefore called “immediate reconstruction”. It allows you to have your mastectomy and to begin your breast reconstruction in one operation. Patients with extensive disease are advised to delay reconstruction until their cancer is firmly in remission.
Step Four:
A pathologist will examine your breast after your lumpectomy or mastectomy. The information provided will allow your oncologist to “stage” your disease so it can be decided how much further treatment you need. If your initial biopsy showed non-invasive cancer, and this was again the only finding after your mastectomy, then you will not need further treatment.
If, however, you are found to have invasive cancer, several factors will be considered to determine if you should have chemotherapy. When a tumor is over 1 inch, has spread to the lymph nodes, or has some other negative biological characteristics such as rapid growth, post-operative chemotherapy is recommended to destroy small groups of cancer cells that may have spread to the rest of your body. This treatment will reduce the risk of your cancer returning. Occasionally, if your tumor is unexpectedly large (over 2 inches) or has spread to more than four lymph nodes, postoperative radiation will be employed, usually following the completion of your chemotherapy.
In summary, the tumor in your breast will be treated with either a lumpectomy and radiation or a mastectomy. Cancer that has spread to your lymph nodes will be identified with a sentinel node biopsy and, when present, will usually be treated with removal of more lymphatic tissue during your mastectomy. Following your mastectomy, the pathologist will analyze all the tissue removed, and the extent of your cancer will be determined or “staged”. If it is felt you have a significant risk of residual cancer elsewhere in your body, chemotherapy will be recommended.
Nipple-Sparing Mastectomy

Breast cancer treatment and prevention by mastectomy has evolved from the disfiguring radical mastectomy to the “Nipple Sparing Mastectomy” (NSM). In this procedure, the entire skin envelop, including the nipple-areola complex (NAC), is preserved, while all of the glandular breast tissue is removed. This reduced disfigurement makes subsequent breast reconstruction simpler and more appealing.
Nipple-sparing mastectomy is based on extensive research that shows there is no increased risk of cancer recurrence, when the procedure is performed on appropriately selected patients. Patients may not be good candidates for NSM if:
- The tumor is near the nipple;
- The tumor involves the skin extensively, as in inflammatory breast cancer;
- The breast is large and/or the nipple is below the breast fold;
- There are previous incisions around the NAC, which can diminish blood flow to the nipple.
Nipple-sparing mastectomy is usually done either through an incision in the fold underneath the breast or through an incision around the bottom half of the areola. The latter excision may need to be extended on the outer aspect of the breast to give the breast surgeon enough room to work. After the breast tissue is removed, the plastic surgeon can proceed with breast reconstruction as he or she would otherwise, only now there is one less part of the breast to replace.
Postoperatively, patients frequently develop discoloration and blistering of the NAC. However, complete loss the the NAC is uncommon. When it does happen, it could require a separate surgery to excise it. Though NSM is a great improvement, it is important to recognize its short comings. Sensation is permanently absent in 100% of patients following the procedure. Likewise, because there is no longer any breast tissue beneath the nipple, breast feeding after is not possible. These last two factors may be more important to women with a genetic predisposition to breast cancer (BRCA 1 & 2) who are considering preventative surgery.
Nipple-sparing mastectomy can make the treatment and prevention of breast cancer less intimidating and allow your reconstructed breast to look more like your own. Please ask your doctor if this procedure is right for you.
Breast Reconstruction Surgery
Once your cancer treatment is complete, it is usually permissible to continue the reconstruction process started at your mastectomy. If you had no reconstruction at the time of your mastectomy, you can begin reconstruction at this point. This can commonly be done within two to three months after finishing chemotherapy. If you also had radiation therapy, it may take longer for your body to be ready for breast reconstruction. The good news is that breast reconstruction surgery is financially your choice. Federal law compels coverage of breast reconstruction following mastectomy. Even procedures on the opposite breast that might be needed to achieve symmetry are covered.
Breast Reconstruction Techniques
The type of reconstruction you choose will depend on your preferences, your body shape, the amount of cancer you seem to have, and the expected treatments you will require.
Oncologic Breast Reconstruction
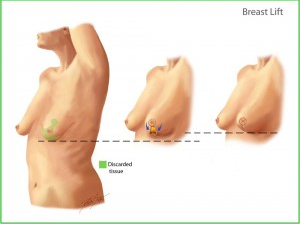
Oncoplastic surgery is a fancy name for a procedure that makes it easier for women with breast cancer to avoid a mastectomy by having a lumpectomy and a breast lift/reduction at the same time.
Normally, a breast cancer can be treated by a lumpectomy only if the tumor is in a good location and is small compared to the size of the breast. If a lumpectomy and radiation is done under non-ideal circumstances, as with a relatively large tumor, the woman’s breast can be permanently deformed. Oncoplastic techniques allow a larger lumpectomy to be performed by the breast surgeon and then the plastic surgeon will sculpt the remaining breast tissue into a normal appearing breast. This is done by performing a breast reduction or lift on the remaining tissue and on the opposite breast to create symmetry.
A breast reduction involves the classic “anchor” incisions: around the areola, down the front of the breast and in the fold beneath the breast. In most cases, sensation to the nipple is preserved. Occasionally, due to a lack of blood supply, the nipple may need to be removed and replaced as a free graft. In these cases, there is a permanent loss of sensation to the nipple.
There are several advantages to Oncoplastic Surgery:
- A breast cancer patient who might otherwise be a bad candidate for keeping her breast can now do so;
- The postoperative radiation is better tolerated in a smaller breast;
- Pre-operative symptoms of breast enlargement are usually relieved;
- It is much safer than trying to "fix" a breast that is distorted following radiation therapy.
This type of procedure is applicable to patients who have extra skin and breast tissue at the time of their cancer diagnosis. Smaller-breasted patients can still have a standard lumpectomy.
Primary Breast Implant
The simplest way to reconstruct a breast is to place an implant immediately after the mastectomy. This is not commonly done for several reasons. For one, it can be difficult to place the implant in the proper position. Secondly, a mastectomy impairs blood flow to the skin. The tense of a primary implant can impair the supply further resulting in skin loss.
Tissue Expansion
Probably the most common form of breast reconstruction in the United States involves the placement of a tissue expander at the time of the mastectomy. Tissue expanders are rubber implants that can be slowly inflated with saline in the plastic surgeon’s office once a patient is healed from her mastectomy. When done patiently, there is little discomfort associated with the expansion, which can take anywhere from several weeks to several months to be completed.
Once the expansion is completed and the patient is done with chemotherapy, an outpatient surgical procedure is performed to replace the expander with either a saline or silicone filled implant. Generally, a new nipple and areola is usually created at the same time, if a nipple-sparing procuedure was not possible. When necessary, procedures to modify the opposite breast in order to attain symmetry are also done at the same time.
A tissue expander placement typically adds less than an hour to the mastectomy procedure. Most of our Dallas breast reconstruction patients are discharged from the hospital within one to two days. Recovery from the second and final procedure is usually rapid, and most patients are able to return to office work within a week. Tissue expander breast reconstruction is relatively simple, safe, and has reliable results, particularly in patients with smaller breasts. This technique does require breast implants, which have a finite life span (90 percent of saline implants last 10 years, silicone implants last closer to 15 years) and can require revision for asymmetry and malposition. Moreover, breast implants placed after tissue expanders have very little tissue coverage, and therefore it can be easy to feel the implant. This form of breast reconstruction is the most common, in part because it is the easiest for the patient and the plastic surgeon. Modern silicone implants have drastically improved the quality of results with this type of reconstruction.
Latissimus Flap Breast Reconstruction
The next type of reconstruction is called a latissimus flap. This operation is like the tissue expander procedure except a muscle from your back with a small piece of skin is placed over the expander. The additional tissue and muscle ultimately makes your reconstructed breast look and feel more natural. The piece of skin is used to replace your nipple and areola is absent, and therefore does a more effective job at preserving your breast shape.
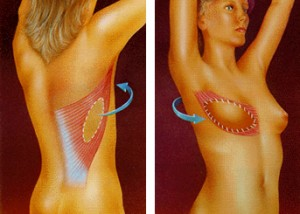 The muscle used in latissimus flap reconstruction is seldom missed even by the most athletic of patients. Recent studies have shown that at one year after surgery, there is no discernible difference in shoulder function. Compared to a tissue expander alone, the hospital stay is usually a day longer on average. After a latissimus flap reconstruction, the reconstructed breast feels much more like a natural breast than one reconstructed with a tissue expander alone.
The muscle used in latissimus flap reconstruction is seldom missed even by the most athletic of patients. Recent studies have shown that at one year after surgery, there is no discernible difference in shoulder function. Compared to a tissue expander alone, the hospital stay is usually a day longer on average. After a latissimus flap reconstruction, the reconstructed breast feels much more like a natural breast than one reconstructed with a tissue expander alone.
Traditional Latissimus Flap
A newer version of this operation is the “Skin-Sparing Latissimus Flap” which offers advantages over the other procedures. Traditionally, a latissimus flap was mostly offered as a breast reconstruction technique to patients who had failed previous attempts. Part of the reason for this was that the flap resulted in two types of deformity, one a long, vertical scar on the back and the second, a large patch of skin on the breast that did not match the surrounding skin in color. The picture in this section demonstrates these problems. Fortunately, over the years, numerous plastic surgeons have modified the latissimus flap so these deformities are now much less of a concern.
It makes sense that in an era of the “Skin-Sparing Mastectomy,” where minimal skin is removed from the breast, the reconstructive procedure should also spare the skin. In a “Skin-Sparing Latissimus (SSL),” the incision is no longer vertical, which heals badly, but transverse, so that it will lie beneath the outline of a woman’s bra. Additionally, since only a woman’s nipple is missing, only a small piece of skin needs to be taken to replace it. This means the back scar is short and ideally, there is no mismatch of skin on the breast as the back skin is later tattooed to become the new areola.
What this means, is that the SSL procedure should be considered for all women undergoing mastectomies who are interested in breast reconstruction. The SSL has some clear advantages over a tissue expander reconstruction or a free-flap reconstruction. An SSL reconstruction frequently employs a tissue expander, but because it uses the patient’s own tissue, the resultant breast usually feels much more normal than a breast reconstructed by an tissue expander alone. In contrast to a free-flap reconstruction, a SSL is much easier for the surgeon to perform and therefore has a much lower failure rate. While the SSL does involve more surgery than an expander alone and does require a breast implant, unlike a free-flap reconstruction, the SSL procedure may be the best choice for breast reconstruction for large number of women undergoing mastectomies.
To understand more about this procedure, go to: http://www.youtube.com/watch?v=3W9uUQRxkJg
Abdominal Flap Breast Reconstruction
It is possible to use excess lower abdominal tissue to reconstruct a breast. Originally, this was called a TRAM flap and the tissue was tunneled into the breast area while still attached to the patient by an abdominal muscle. This muscle would supply blood to the flap and was called its “pedicle”. Though dramatic results are possible with a “pedicled TRAM,” it is not commonly performed due to a propensity for serious complications such as chronic pain, abdominal hernias, and loss of the tissue.
The TRAM flap has been modified many times, so now the lower abdominal tissue can be transplanted to the breast with little or no muscle being sacrificed, making abdominal weakness less of an issue. These operations now require the surgeon to use microsurgery to reconnect small blood vessels supplying the abdominal tissue to other vessels in the chest to make the transplantation successful. The DIEP flap is the most common example of this type of surgery. Due to the complexity of the procedure, it will usually be performed in about 8 hours when done on both sides. These times vary tremendously with the skill and experience of the plastic surgeon. The advantage of this operation is that the breast is reconstructed with your own tissue. The major disadvantage is that between 5 to 10 percent of the time, the entire operation fails and another avenue must be pursued. Such a loss is particularly devastating for patients who are already struggling with their new diagnosis of breast cancer and its treatment. Since Dr. Pin does not perform microvascular surgery, he does not do breast reconstruction with abdominal flaps; if you are interested in this procedure, Dr. Pin will try to help you find a surgeon who does.
Before and After Photos
Featured Cases

Latissimus Flap and Implant Reconstruction
This 34-year-old woman was found to have a gene that causes breast cancer (BRCA.) Due to a very high risk of developing breast cancer, she elected to have both breasts removed w
+ See Full Case
Nipple Sparing Mastectomy
This patient was a 27 year old with the BRCA 1 gene mutation who decided to have bilateral "nipple sparing" mastectomies.
+ See Full Case
Partial Mastectomy with Oncoplastic Breast Reconstruction
This 48-year-old woman was 5'5", 170 pounds,and had a small right breast cancer in the setting of her breast hypertrophy. This case is particularly interesting for a couple of
+ See Full CaseLatissimus Flap and Implant Reconstruction
This 34-year-old woman was found to have a gene that causes breast cancer (BRCA.) Due to a very high risk of developing breast cancer, she elected to have both breasts removed with simultaneous latissimus flaps and tissue expanders. At a second stage, she had silicone implants placed and had nipple areolar reconstruction.
Nipple-sparing Mastectomy
This patient was a 27 year old with the BRCA 1 gene mutation who decided to have bilateral “nipple sparing” mastectomies. She underwent bilateral mastectomies with tissue expander placement. She had permanent silicone implants placed three months later.
Partial Mastectomy With Oncoplastic Breast Reconstruction
This case is particularly interesting for a couple of reasons. First, the patient had a partial mastectomy. Second, she underwent breast reconstruction using a breast reduction pattern. Because it is used in the setting of cancer treatment, it is called “Oncoplastic.” Note in the Before picture that her breasts are large and droopy, to the point that the nipple has fallen below the line of the inframammary crease (the point at which the underside of the breast meets the chest wall). The After photo shows that her breasts have been reduced in size and lifted so that the nipples point forward. This technique is useful for the breast cancer patient who has a small tumor compared to the size of her breast, who has large breasts and who desires to have breast conservation instead of a mastectomy.
Although being diagnosed with breast cancer or as a carrier for the mutant BRCA gene may be traumatic, there are many techniques that can be used to reconstruct the breasts and allow women to regain some confidence and healing in their lives.
Shortcomings of Reconstruction
Breast reconstruction has the obvious benefit of allowing a woman to feel whole after a mastectomy. Nevertheless, there are drawbacks. Breast reconstruction, no matter how well planned and executed, will always involve at least some permanent scarring. Due to the mastectomy, the sensation of your breast will never be normal, though hopefully over time the numbness may be less perceptible. Regardless of the technique used, there will always be some degree of asymmetry between your breasts, both in terms of volume and feel. Finally, there are the risks associated with any surgical procedure such as bleeding, infection, and delayed healing. Sometimes, additional surgery is needed to treat these complications. The probability of these risks is related to your general health, whether you are overweight, and whether you smoke. Dr. Pin tries not to do breast reconstruction on patients until they completely stop smoking because the complications from smoking can be devastating and irreparable.
Being a breast cancer patient can be extremely difficult. There is so much information to absorb and so many new terms to learn while somehow dealing with emotions ranging from fear to anger to confusion. The good news is you are not alone. You will find strength in family and friends and, most surprisingly, in yourself. During your treatment, you will be amazed by your own determination. When you complete your treatment, you will know a new sense of accomplishment. You will be stronger, more compassionate, and more understanding than you are now. But, most of all, you will be proud of yourself!
Dallas Breast Reconstruction Consultations
Contact our Dallas office to schedule your breast reconstruction consultation with us.
Surgery for breast reconstruction is real surgery and involves risks such as bleeding, infection, and scarring. Results vary. Dr. Pin will be happy to discuss these and other risks of surgery for breast reconstruction.
